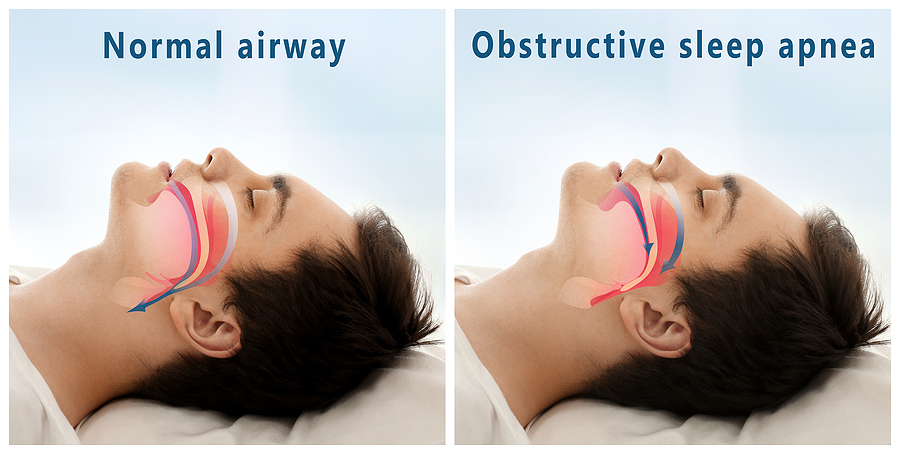
Obstructive Sleep Apnea (OSA) Treatment Options for Pilots – Obstructive Sleep Apnea affects approximately 30% of adult males and 15% of adult females in North America [1]. Those with risk factors such as obesity, large neck circumference, or a family history of sleep disorders are at even greater risk. If you are a heavy snorer, wake up with headaches, sore throat, or dry mouth, or don’t feel rested in the morning, there is a good chance you might be suffering from sleep apnea.
But OSA is more than just snoring and poor sleep—it is strongly associated with severe comorbid conditions like hypertension, cardiovascular disease, type 2 diabetes, obesity, mood disorders, and cognitive impairment.
Given these health consequences, it is understandable that the FAA considers OSA a public safety issue and instructs Aviation Medical Examiners (AMEs) to at least consider the diagnosis during each FAA medical examination.
FAA Policy: Myths vs. Reality
Because OSA is so common, the FAA developed a streamlined protocol to allow for faster certification decisions, particularly when pilots are proactive and compliant with treatment [2]. In fact, as of May 2025, OSA is the only medical condition that requires a special issuance but does not require AMEs to defer your application or seek special permission from the FAA to issue a certificate.
Even so, many pilots who suspect they have OSA still do not address it with their doctors. There is a widespread, persistent belief that an OSA diagnosis will lead to months-long delays or permanent grounding.
In fact, pilots who provide their AMEs with the correct documentation can leave the office with their medical certificate in hand, without waiting for the FAA.
OSA Treatment Options for Pilots
The key to successfully navigating the process lies in proper diagnosis, selecting a treatment option that meets the FAA’s certification requirements, and providing the correct documentation to support your cause. This is where many pilots—and doctors—get confused.
Positive airway pressure is the “gold standard” for OSA treatment. It involves using a machine that pushes air through a mask with enough force to prevent your throat from closing while you sleep.
For those who need it, PAP can be life-changing, but many pilots with milder forms of sleep apnea are reluctant to commit to PAP-based therapy unless absolutely required. In fairness, the tubes, masks, humidifiers, filters, and cleaning requirements that come with it can be a big adjustment.
For those with mild OSA, oral devices, positional therapy, and even observation (no treatment at all) can be acceptable alternatives, provided that your sleep study was sufficiently sensitive to rule out moderate or severe disease.
Diagnosis: Type I and Type II Sleep Studies
More and more sleep specialists are using home-based studies to diagnose sleep apnea. The tests are low-cost, relatively accurate, and easy enough for patients to administer at home. Unfortunately, they also tend to miss some cases of OSA entirely and miscategorize other cases as being milder than they actually are.
As you can imagine, these low-fidelity sleep tests (e.g., Type III or IV) do not meet FAA requirements for diagnostic or post-treatment verification purposes [3].
For FAA certification purposes, diagnosis of OSA must be made using a Type I or Type II sleep study:
- Type I Sleep Study: Conducted in a sleep lab, includes full polysomnography with technician monitoring.
- Type II Sleep Study: Conducted at home using portable monitoring equipment, but still meets medical diagnostic standards.
Treatment Options Based on AHI Categories
The sleep study results in an AHI score, which measures how many apnea (complete cessation of airflow) and hypopnea (partial obstruction) events occur per hour of sleep. As long as you had a Type I or II sleep study, the FAA uses this index to determine acceptable treatment pathways.
AHI ≥ 16: PAP Therapy Is Mandatory
For any airman with a baseline AHI of 16 or higher, Positive Airway Pressure (PAP) therapy is required. This includes CPAP (Continuous Positive Airway Pressure) and APAP (Automatic PAP) machines, which maintain an open airway during sleep.
AHI Between 10 and 15.9: Alternatives Possible, But Follow-Up Required
For AHI scores in the 10.0 to 15.9 range, the FAA allows alternative treatments like oral appliances (custom dental devices) or positional therapy, but only after follow-up verification.
A Type I or II sleep study must be repeated while using the prescribed treatment to demonstrate that the AHI has been reduced to below 10. Without this proof, the treatment will not be accepted by the FAA, even if you feel better.
AHI < 10: Alternatives Without Additional Testing
If the pilot’s baseline AHI is below 10, treatment is still encouraged if symptoms persist, but FAA requirements are more relaxed. Dental appliances or positional therapy are permitted at the physician’s discretion, and no follow-up sleep study is required if symptoms improve.
Non-Type I or II Sleep Studies
You can still qualify for a special issuance if your OSA was diagnosed with a lower-quality sleep study, but only if you are treated with PAP. Before you begin any other form of treatment as a pilot, you must make sure your most recent diagnostic sleep study was a Type I or II study.
Otherwise, you could face significant delays in your medical certification.
Changing OSA Treatment
As long as your most recent Type I or II sleep study and your treating doctor support it, you can change treatment methods whenever you like. The FAA uses somewhat ambiguous language on this point in their special issuance instructions, but they allow a surprising level of flexibility.
Whether you opted for PAP treatment even though it was not required or your AHI went down due to weight loss or surgery, the treatment options available to you under the FAA’s certification protocol are always based on your AHI on your most recent Type I or II study.
Documentation for FAA Compliance
For a smooth FAA certification process, make sure to gather all required documentation before you schedule an appointment with your AME. Technically, your AME can issue your certificate following a new OSA diagnosis even if you do not provide the required documents, but many feel uncomfortable accepting that level of risk. The documents the FAA requires are:
- Most recent diagnostic sleep study results. If you intend to use a treatment other than PAP, you must have a Type I or II study.
- Follow-up sleep study, if applicable (for AHI 10–15.9 and non-PAP treatment). This must also be a Type I or II study.
- Treatment compliance report. This applies most commonly to PAP treatment, but if your dental device or other treatment device supports compliance monitoring, you must include the associated data.
- Status report from the treating physician to verify ongoing treatment and stability. The FAA publishes standardized forms for this purpose.
- Pilot’s signed statement of treatment compliance (for initial special issuance application)
While the FAA may allow up to 90 days from your exam or their request to provide these documents, we highly recommend that you prepare them before your AME appointment and offer them as soon as possible after your exam. Failure to do so could result in suspension or non-issuance of the certificate.
Even better, talk to your AME before your exam. Some AMEs are more familiar with FAA policy than others. Having an informed discussion upfront can prevent misunderstandings or unnecessary deferrals.
Managing OSA Without Compromising Your Medical Certificate
OSA is common, manageable, treatable, and DOES NOT threaten your FAA medical as long as it is well managed. Most pilots with OSA can maintain their FAA medical certificate without interruption. The key lies in proper diagnosis, selecting a treatment plan that meets the FAA’s requirements, and complete documentation.
Many pilots also have the option to explore different treatment options without first asking the FAA for permission. Ensure you, your treating physician, and your AME fully understand the FAA’s protocol before changing your treatment plan.
# Obstructive Sleep Apnea (OSA) Treatment Options for Pilots
References
[1] T. Young, M. Palta, J. Dempsey, P. E. Peppard, F. J. Nieto, and K. M. Hla, “Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study,” WMJ, vol. 108, no. 5, pp. 246–249, Aug. 2009.
[2] Federal Aviation Administration, “Decision Considerations Disease Protocols – Obstructive Sleep Apnea (OSA),” [Online]. Available: https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/dec_cons/disease_prot/osa/. [Accessed: Nov. 02, 2021].
[3] American Academy of Sleep Medicine, “Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea,” J. Clin. Sleep Med., vol. 13, no. 3, pp. 479–504, 2017.
[4] D. P. White et al., “Obstructive Sleep Apnea: Definitions, Epidemiology & Natural History,” Respir. Care, vol. 55, no. 9, pp. 1155–1162, Sep. 2010.